Sickle Cell Anemia, What Is It?
By: Najaam Lee/ www.NajaamLee.com
Rastafari.TV
I get this question a lot, what is Sickle Cell? Because the statement that rolls out after is ” You don’t look sick! “. At times, depending on the day and mood, this statement can be taken as a negative or a positive. My question to them would be, ” What does sick look like? “, because this is part of the norm for many people living with Sickle Cell or SS, including myself.
In this article I’m going to break down the definition of Sickle Cell Anaemia, and discuss what it is and isn’t, how did it come to past, and how it affects the body and lifestyle of one’s living with SS.
What is Sickle Cell Anemia?
According to https://www.medicinenet.com/sickle_cell/article.htm
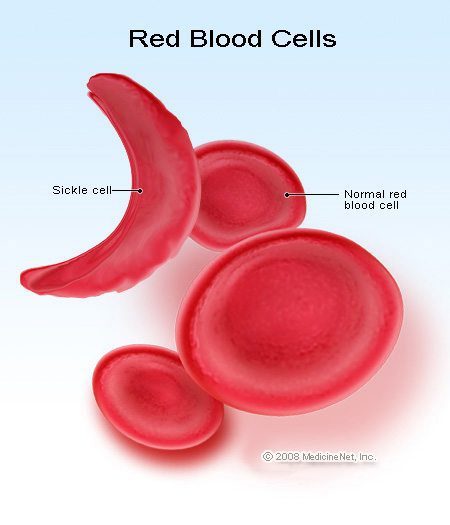
Sickle cell anemia (sickle cell disease) is a disorder of the blood caused by an inherited abnormal hemoglobin (the oxygen-carrying protein within the red blood cells). The abnormal hemoglobin causes distorted (sickled) red blood cells. The sickled red blood cells are fragile and prone to rupture. When the number of red blood cells decreases from rupture (hemolysis), anemia is the result. This condition is referred to as sickle cell anemia. The irregular sickled cells can also block blood vessels causing tissue and organ damage and pain.
Sickle cell anemia is one of the most common inherited blood anemias. The disease primarily affects Africans and African Americans. It is estimated that in the United States, some 90,000 to 100,000 Americans are afflicted with sickle cell anemia. Overall, current estimates are that one in 500 U.S. African American births is affected with sickle cell anemia.
Also please note, Sickle Cell is not only an African American disease, other countries such as Africa, India, the Mediterranean, Saudi Arabia, and South and Central America. In the United States, it most commonly affects African Americans and Hispanics, but the US is a melting pot with other nations here living with SS. There are many types of Sickle Cell which I will break down for you:
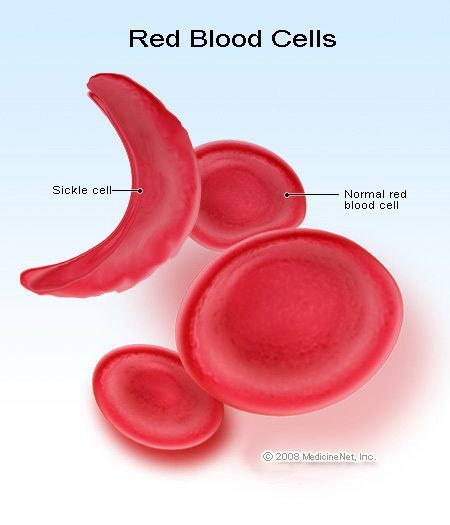
Credit: MedicineNet.com
Reference: St. Jude, https://www.stjude.org/stjude/v/index.jsp?vgnextoid=1141ef5d00670110VgnVCM1000001e0215acRCRD
Hemoglobin SS, Hemoglobin SC, and Sickle Beta Thalassemia are the most common types of sickle cell disease.
-
Hemoglobin SS is homozygous sickle cell disease. The hemoglobin S gene is inherited from both parents.
-
Hemoglobin SC is heterozygous sickle cell disease. Hemoglobin S is inherited from one parent and hemoglobin C is inherited from the other parent.
-
Sickle Beta Thalassemia is heterozygous sickle cell disease. Hemoglobin S is inherited from one parent and the beta thalassemia gene is inherited from the other parent.
Related Facts:
-
The sickle cell gene is caused by a mutation in the hemoglobin gene.
-
Hemoglobin is the part of the red blood cell that carries oxygen.
-
Normal hemoglobin is hemoglobin A.
-
Sickle hemoglobin is hemoglobin S.
-
Hemoglobin S is an abnormal type of hemoglobin.
-
Most people with sickle cell disease do not have normal hemoglobin.
As a Sickler myself, I carry the full disease, Hemoglobin SS. Living with SS, I incur painful crises or Sickle Cell attacks, anywhere in my body, at any given time. Most prominent areas are the back, stomach, chest and legs. Now, when people hear about a person with SS, automatically assumptions and advice are immediately given, such as:
– ” You need to eat more!
– ” You need good food in your belly.”
– ” you must get up and move. You not doing enough for your body”
Trust me, I have heard it all, and this is based off ignorance. Your eating, food, movement, etc will not stop or prevent a Sickle Cell Attack! Let’s be clear. We, sicklers, are dealing with an illness that is invisible to the naked eye, so how we move with this disease is on another level.
Reference: https://www.medicinenet.com/sickle_cell/page2.htm#what_conditions_promote_the_sickling_of_the_red_blood_cells
What conditions promote the sickling (distortion) of the red blood cells in sickle cell anemia?
Sickling of the red blood cells in patients with sickle cell anemia results in cells of abnormal shape and diminished flexibility. The sickling is promoted by conditions which are associated with low oxygen levels, increased acidity, or low volume (dehydration) of the blood. These conditions can occur as a result of injury to the body’s tissues, dehydration, or anesthesia.
Certain organs are predisposed to lower oxygen levels or acidity, such as when blood moves slowly through the spleen, liver, or kidney. Also, organs with particularly high metabolism rates (such as the brain, muscles, and the placenta in a pregnant woman with sickle cell anemia) promote sickling by extracting more oxygen from the blood. These conditions make these organs susceptible to injury from sickle cell anemia.
So lets get in depth about Sickle Cell Symptoms. There is NO CURE. There are only treatments available. And not enough research. We need more Research Doctors or Scientists to fully dedicate to the finding a cure and are BOLD enough to push through the Politics that surround this disease. Yes, what has been stopping main stream research for Sickle Cell, is the politics, which holds back a lot of the funding needed. As you will see, most of the treatments suggested for Sickle Cell patients are coming from Cancer research and trials, and is passed on to us to try out or use such as Hydroxyurea . We need people on the floors of government to push and make these changes happen.
Reference: https://www.medicinenet.com/sickle_cell/page3.htm
What are the symptoms and treatments of sickle cell anemia?
Virtually all of the major symptoms of sickle cell anemia are the direct result of the abnormally shaped, sickled red blood cells blocking the flow of blood that circulates through the tissues of the body. The tissues with impaired circulation suffer damage from lack of oxygen. Damage to tissues and organs of the body can cause severe disability in patients with sickle cell anemia. The patients endure episodes of intermittent “crises” of variable frequency and severity, depending on the degree of organ involvement.
The major features of sickle cell anemia include:
- Fatigue and Anemia
- Pain Crises
- Dactylitis (swelling and inflammation of the hands and/or feet) and Arthritis
- Bacterial Infections
- Splenic Sequestration (sudden pooling of blood in the spleen) and Liver Congestion
- Lung and Heart Injury
- Leg Ulcers
- Aseptic Necrosis and Bone Infarcts (death of portions of bone)
- Eye Damage
- Other Features
Some features of sickle cell anemia, such as fatigue, anemia, pain crises, and bone infarcts can occur at any age. Many features typically occur in certain age groups.
Sickle cell anemia usually first presents in the first year of life. Infants and younger children can suffer with fever, abdominal pain, pneumococcal bacterial infections, painful swellings of the hands and feet (dactylitis), and splenic sequestration. Adolescents and young adults more commonly develop leg ulcers, aseptic necrosis, and eye damage. Symptoms in adult typically are intermittent pain episodes due to injury of bone, muscle, or internal organs.
Affected infants do not develop symptoms in the first few months of life because the hemoglobin produced by the developing fetus (fetal hemoglobin) protects the red blood cells from sickling. This fetal hemoglobin is absent in the red blood cells that are produced after birth so that by 5 months of age, the sickling of the red blood cells is prominent and symptoms begin.
The treatment of sickle cell anemia is directed to the individual features of the illness present. In general treatment is directed at the management and prevention of the acute manifestations as well as therapies directed toward blocking the red blood cells from stacking together. There is no single remedy to reverse the anemia. It is, therefore, important that affected individuals and their family members have an optimal understanding of the illness and that communication with the doctors and medical personnel be maintained.
Fatigue and Anemia
Fatigue is a common symptom in persons with sickle cell anemia. Sickle cell anemia causes a chronic form of anemia which can lead to fatigue. The sickled red blood cells are prone to breakage (hemolysis) which causes reduced red blood cell life span (the normal life span of a red blood cell is 120 days). These sickled red blood cells are easily detected with a microscope examination of a smear of blood on a glass slide.
Typically, the site of red blood cell production (bone marrow) works overtime to produce these cells rapidly, attempting to compensate for their destruction in the circulation. Occasionally, the bone marrow suddenly stops producing the red blood cells which causes a very severe form of anemia (aplastic crises). Aplastic crises can be promoted by infections that otherwise would seem less significant, including viruses of the stomach and bowels and the flu (influenza).
The anemia of sickle cell anemia tends to stabilize without specific treatments. The degree of anemia is defined by measurement of the blood hemoglobin level. Hemoglobin is the protein molecule in red blood cells which carries oxygen from the lungs to the body’s tissues and returns carbon dioxide from the tissues to the lungs. Blood hemoglobin levels in persons with sickle cell anemia are generally between 6 to 8 gms/dl (normal levels are above 11 gms/dl). Occasionally, there can be a severe drop in hemoglobin requiring a blood transfusion to correct the anemia (such as in patients suffering splenic sequestration). Blood transfusion is usually reserved for those patients with other complications, including pneumonia, lung infarction, stroke, severe leg ulceration, or late pregnancy. (Among the risks of blood transfusion are hepatitis, infection, immune reaction, and injury to body tissues from iron overload.) Transfusions are also given to patients to prepare them for surgical procedures. Folic acid is given as a supplement.
Pain Crises
Pain crises in persons with sickle cell anemia are intermittent painful episodes that are the result of inadequate blood supply to body tissues. The impaired circulation is caused by the blockage of various blood vessels from the sickling of red blood cells. The sickled red blood cells slow or completely impede the normal flow of blood through the tissues. This leads to excruciating pain, often requiring hospitalization and opiate medication for relief. The pain typically is throbbing and can change its location from one body area to another. Bones are frequently affected. Pain in the abdomen with tenderness is common and can mimic appendicitis. Fever frequently is associated with the pain crises.
A pain crisis can be promoted by preceding dehydration, infection, injury, cold exposure, emotional stress, or strenuous exercise. As a prevention measure, persons with sickle cell anemia should avoid extremes of heat and cold.
Pain crises require analgesia for pain and increased fluid intake. Dehydration must be prevented to avoid further injury to the tissues and intravenous fluids can be necessary. Along with the fluids clotrimazole and magnesium are often given. Other modalities, such as biofeedback, self-hypnosis, and/or electrical nerve stimulation may be helpful.
Hydroxyurea is a medication that is currently being used in adults and children with severe pain from sickle cell anemia. It is also considered for those with recurrent strokes and frequent transfusions. This drug acts by increasing the amount of fetal hemoglobin in the blood (this form of hemoglobin is resistant to sickling of the red blood cells). The response to hydroxyurea is variable and unpredictable from patient to patient. Hydroxyurea can be suppressive to the bone marrow.
Dactylitis and Arthritis
Swelling and inflammation of the hands and/or feet is often an early sign of sickle cell anemia. The swelling involves entire fingers and/or toes and is called dactylitis. Dactylitis is caused by injury to the bones of the affected digits by repeated episodes of inadequate blood circulation. Dactylitis generally occurs in children with sickle cell anemia from age 6 months to 8 years.
Joint inflammation (arthritis) with pain, swelling, tenderness, and limited range of motion can accompany the dactylitis. Sometimes, not only the joints of the hands or feet are affected, but also a knee or an elbow.
The inflammation from dactylitis and arthritis can be reduced by anti-inflammation medications, such as ibuprofen and aspirin.
Bacterial Infection
Lung infection (pneumonia) is extremely common in children with sickle cell anemia and is also the most common reason for hospitalization. Pneumonia can be slow to respond to antibiotics. The type of bacteria that is frequently the cause of pneumonia is called the pneumococcus. (This is, in part, due to the increased susceptibility to this particular bacteria when the spleen is poorly functioning.) Vaccination against pneumococcal infection is generally recommended.
Children with sickle cell anemia are also at risk for infection of the brain and spinal fluid (meningitis). Bacteria that are frequent causes of this infection include the Pneumococcus and Haemophilus bacteria.
Furthermore, children with sickle cell anemia are at risk for an unusual form of bone infection (osteomyelitis). The infection is typically from a bacteria called Salmonella.
Bacterial infections can be serious and even overwhelming for patients with sickle cell anemia. Early detection and antibiotic treatment are the keys to minimizing complications. Any child with sickle cell anemia must be evaluated by medical professionals when fever or other signs of infection (such as unexplained pain or cough) appear.
Splenic Sequestration and Liver Congestion
It has been demonstrated that the liver, and especially the spleen, are organs that are very active in removing sickled red blood cells from the circulation of persons with sickle cell anemia. This process can accelerate suddenly. Sudden pooling of blood in the spleen is referred to as splenic sequestration.
Splenic sequestration can cause very severe anemia and even result in death.
The spleen is commonly enlarged (splenomegaly) in younger children with sickle cell anemia. As the spleen is repeatedly injured by damage from impaired blood supply, it gradually shrinks with scarring. Impairment of the normal function of the spleen increases the tendency to become infected with bacteria.
Sudden pooling of blood in the spleen (splenic sequestration) can result in a very severe anemia and death. These patients can develop shock and lose consciousness. Transfusion of blood and fluids can be critical if this occurs.
Liver enlargement (hepatomegaly) occurs as it becomes congested with red blood cells as well. The liver is often firm and can become tender. Impaired liver function can result in yellowing of the eyes (jaundice). The gallbladder, which drains bile from the liver, can fill with gallstones. Inflammation of the gallbladder (cholecystitis) can cause nausea and vomiting and require its removal.
Lung and Heart Injury
Aside from lung infection (pneumonia), the lungs of children with sickle cell anemia can also be injured by inadequate circulation of blood which causes areas of tissue death. This lung damage can be difficult to distinguish from pneumonia and is known as acute chest syndrome. These localized areas of lung tissue damage are referred to as pulmonary infarcts. Pulmonary infarcts often require a special x-ray test using a dye injected into the affected areas (angiogram) for diagnosis. Repeated pulmonary infarcts can lead to scarring of the lungs of children with sickle cell anemia by the time they reach adolescence.
The heart is frequently enlarged in children with sickle cell anemia. Rapid heart rates and murmurs are common. The heart muscle can also be injured by infarcts and iron depositing in the muscle as it leaks from the ruptured red blood cells.
Injuries to the lungs or heart are treated according to the specific type of damage and the degree of impairment of organ function. Supplementary oxygen can be required. Infections of the lungs require aggressive antibiotics. Transfusions can sometimes help prevent further damage to the lung tissue. Heart failure can require medications to assist the heart in more effectively pumping blood to the body.
Leg Ulcers
The legs of patients with sickle cell anemia are susceptible to skin breakdown and ulceration. This seems to be a result of the stagnant blood flow caused by the sickled red blood cells. Injury to the skin of the legs or ankles can promote skin damage and ulceration.
Leg ulcers most commonly occur in adults and usually form over the ankles and sides of the lower legs. The ulcers can become severe, even encircling the leg, and are prone to infection.
Leg ulcers can become chronic and resistant to many treatments. Oral antibiotics and topical creams are often used. Elevation of the leg, careful dressing changes, and other topical therapies can be helpful. Some ulcers can be so resistant that skin grafting is recommended, though this may be compromised by impaired healing.
Aseptic Necrosis and Bone Infarcts
Inadequate circulation of the blood, which is characteristic of sickle cell anemia, also causes areas of death of bone tissue (bone infarction). Aseptic necrosis, or localized bone death, is a result of inadequate oxygen supply to the bone. Aseptic necrosis is also referred to as osteonecrosis.
While virtually any bone can be affected, the most common are the bones of the thighs, legs, and arms. The result can permanently damage or deform the hips, shoulders, or knees. Pain, tenderness, and disability frequently are signs of aseptic necrosis. Painful bone infarcts can be relieved by rest and pain medications.
Aseptic necrosis can permanently damage large joints (such as the hips or shoulders). Local pain can be relieved and worsening of the condition can be prevented by avoiding weight bearing. With more severe damage, total joint replacement may be needed to restore function.
Eye Damage
The critical area of the eye that normally senses light is called the retina. The retina is in the back of the eye and is nourished by many tiny blood vessels. Impairment of the circulation from the sickling of red blood cells results in damage to the retina (retinopathy). The result can be partial or complete blindness.
Bleeding can also occur within the eye (retinal hemorrhage) and retinal detachment can result. Retinal detachment can lead to blindness.
Once blindness occurs, it is usually permanent. Preventative measures, such as laser treatments, can be used if bleeding into the eye and retinal detachment are detected early.
Other Features
Additional features of sickle cell anemia include weakening of bones from osteoporosis, kidney damage and infection, and nervous system damage. Osteoporosis can lead to severe pain in the back and deformity from collapse of the spine (vertebrae). Kidney damage can lead to poor kidney function with a resulting imbalance of blood sodium and acidity as well as bleeding into the urine. Kidney infection can cause pelvic pain and require hospitalization with antibiotic treatment. Injury to the nervous system can result from meningitis or sickle cell anemia itself. Poor blood circulation in the brain can cause stroke, convulsions, and coma.
Damage to the brain from stroke can cause permanent loss of function to areas of the body. Transfusion of blood and fluids intravenously can be critical. Medications to reduce the chance of seizures are sometimes added. If stroke results in long-term impairment of function, physical therapy, speech therapy, and occupational therapy can be helpful.
Priapism, an abnormally persistent erection of the penis in the absence of sexual desire, can occur in persons with sickle cell anemia. Priapism can lead to impotence and damage to affected tissues.
The big question that is asked is, How Long Will I Live? Death is going to happen regardless if I had Sickle Cell or not. But, because I do live with SS, my life expectancy has shortened tremendously. Most living with SS will live up to the age of 40. But there are some lucky ones who have outlived that number, such as myself, woohoo. And these lucky ones may live up to the age of 60 or less. So let me break it down further,
Reference: https://www.medicinenet.com/sickle_cell/page4.htm
What is the outlook (prognosis) for patients with sickle cell anemia?
The life expectancy of persons with sickle cell anemia is reduced. Some patients, however, can remain without symptoms for years, while others do not survive infancy or early childhood. Nevertheless, with optimal management patients can now survive beyond the fourth decade.
Most patients suffer intermittent pain crises, fatigue, bacterial infections, and progressive tissue and organ damage. Impaired growth and development is the end result of the physical and emotional trauma that is endured by children with sickle cell anemia.
Causes of death include bacterial infection (the most common cause), stroke or bleeding into the brain, and kidney, heart, or liver failure. The risk of bacterial infections does diminish after three years of age. Nevertheless, bacterial infections are the most common cause of death at any age. Therefore, any signs of infection in a person with sickle cell anemia must be reviewed with a doctor to prevent damage and save lives.
Interestingly, the sickle cell gene somewhat protects against malaria infection. This makes those with sickle cell trait (gene carriers) at least partially resistant to malaria. Furthermore, the geographic distribution of the sickle cell gene is similar to that of malaria infection. Sickle cell anemia is a lethal condition that threatens life. But there may be a selective advantage to being a sickle cell carrier (trait) if the person resides in an area of the world where malaria is very common. The advantage a person with sickle cell trait has over a non-carrier of the gene may explain why sickle cell anemia did not disappear from the world even though it is lethal.
The sickle cell gene is not a “black gene.” It just happens to disproportionately occur in the black population. When a black person who carries a sickle cell gene has children with a non-black person, the children may inherit the sickle cell gene regardless of race. There are also people of all races who carry the sickle cell gene.
Recent research is examining further ways to promote the development of the fetal hemoglobin that delays the development of sickle cell in the newborn. Bone marrow transplantation is being used for patients with severe sickle cell anemia who have a sibling donor. Future treatments may involve genetic engineering where cures might be achieved.
Finally, genetic counseling can be helpful for parents and families to prevent sickle cell anemia. Sickle cell anemia is an inherited illness. Both parents must be carriers of the sickle cell gene for a child to be affected with sickle cell anemia. If each parent is a carrier, any child has a one chance in two (50%) of also being a carrier and a one in four (25%) chance of inheriting both genes from the parents and being affected with sickle cell anemia.
Medically reviewed by David Hoffman, MD; American Board of Internal Medicine with subspecialties in Oncology and Hematology
REFERENCE:
Bunn, HF. Pathogenesis and treatment of sickle cell disease. N Engl J Med 1997; 337:762.
Harrison’s Principles of Internal Medicine, McGraw-Hill, edited by Eugene Braunwald, et. al., 2001.
The best thing about living with Sickle Cell is that it has opened my mind to understanding the physical body in a deep way and has connected me spiritually to see beyond the veil that exist around us all. Knowing that there is more to come after this particular life has enlightened me and enriched my life. Therefore, no need for a pity party, what is needed is support, understanding and to have an open-mind. If you carry these qualities, then we can work together in finding the best cure.
Namaste,
Najaam Lee

Credit: NL Art Studios